Essential point-of-care tests for veterinarians, part 1: The aFAST3 scan


Spice up your imaging skills with aFAST3 exams.
aFAST3 scans or (abdominal) focused assessment for sonography trauma scans help identify fluid, fluid, and yup, fluid. But the skill also allows the identification of much more, aiding in your assessment and diagnostic capabilities for your patients.
Why all the buzz about aFAST3 scans?
AFAST scans came about as a result of extrapolation from human medicine. Initially developed for the assessment after blunt force trauma, FAST scans showed high sensitivity in diagnosing abdominal hemorrhage. Over time these scans proved fruitful in veterinary medicine and developed into more than just trauma assessments.
The origins of aFAST examinations and the relevance of the superscript
A 2004 prospective study by Boysen et al. found a 96% sensitivity with 100% specificity for abdominal effusion detection by ultrasound. The study evaluated 100 hit-by-car dogs with blunt force trauma.5,6
Lisciandro1,2 described the initial techniques and started utilizing the scans in 2004. By 2009, these exams received veterinary validation for blunt force trauma. However, in 2014, the removal of the trauma focus brought about the use of the superscript.
This number 3 superscript provides an important update in the emphasis of the scans to include: trauma, triage, and tracking.
Originally, these scans were used primarily in the emergency and critical care setting. But over time, their utility for non-emergent and emergent situations, as well as for tracking progress to therapy over time, for fluid overload assessment, and other applications became evident.
Today, in 2022, these scans have a place in day-to-day practice and are becoming an important standard of care. Failure to acknowledge the aFAST3‘s recognized value as a diagnostic tool could soon leave you open to liability for not keeping up with this level of care.
Thus, there is no reason why you can’t learn the skill and implement it in practice. It isn’t just for emergency and critical care use any longer.
Want more clinical and industry news from IndeVets? Sign up here.
Benefits of aFAST3 scans
Various authors3–5 note that when evaluating for ascites, an aFAST3 scan demonstrates up to twice the sensitivity vs. radiographs, especially when assessing fluid levels ≤ 2 ml/kg. At least 9ml/kg of fluid must be present to be identified radiographically.
However, the benefits of this exam go beyond the ability to easily detect small abdominal effusions. You can bring the machine to the patient for stressed, critical, dyspneic, or anxious patients, minimizing patient stress and anxiety.
It can be done with owners present to demonstrate findings, making it real for them. Additionally, minimal, if any, patient manipulation is needed, unlike traditional radiography.
When should you use an aFAST3 scan?
Of course, nothing replaces your physical exam, the clinical history, and the overall impression of the patient. But we can all use assistance in coming to our diagnosis. An aFAST scan can be performed in 2 minutes or less and can easily help you decide your next steps.
In an emergency scenario, an aFAST scan provides a quick evaluation to assess for the presence of abdominal fluid. Once evaluated, knowing if fluid is present or absent helps to guide fluid resuscitation and diagnostics such as abdominocentesis.
Initially designed to give a yes or no fluid answer, it isn’t designed for extensive abdominal examination. However, over time, clinicians have recognized its utility. They have honed skills and techniques to gleam more than just if fluid is present or absent.
Sure, various emergency scenarios smack you upside the head saying, I should scan the belly for free fluid, or I should see if there is a mass. Clinical signs such as short, shallow, rapid breathing, exercise intolerance, weakness or acute collapse, syncope, abdominal distension, and vomiting come to mind.
However, more vague signs such as lethargy or just a decreased appetite in combination with a signalment, say of a 14-year-old DSH or a 12-year-old Golden Retriever, may need that probe just as much as the respiratory distress patient.
I cannot tell you how many times a weak or exercise intolerant large breed dog has come in with no evidence of dyspnea, vomiting, diarrhea, or other overtly recognizable clinical signs, and they have tricavital effusion.
Some patients are subtle and hide signs, while others, like many cats, don’t like to present in typical fashions. But having the ability to perform an aFAST scan and the confidence in that skill could make the difference between life or death for that patient.
What can one identify on an aFAST3 scan?
We can identify a fair amount in a brief scan. While some of the problems we may discover will be obvious, others will require some extra training on your part to learn some of the tricks of the ultrasound trade. But knowing the basics for the scan and regular practice can help you to acquire that proficiency. You could detect
- Fluid, fluid, and fluid
- Abdominal masses such as a splenic mass
- Pyometra
- Bladder stones
- Pancreatitis
- Gallbladder disease
- Anaphylaxis
More from Dr. Tramuto-Drobnis: Everything you wanted to know about monkeypox and vet med
What you all want to know – The scanning technique
When scanning a patient, hold your probe longitudinally. I usually keep the ultrasound logo on the left of the screen. Regardless, you want the transducer notch (marker) facing the patient’s head on the long axis, then rotate the probe 90 degrees as needed as you scan.7,8(p3)
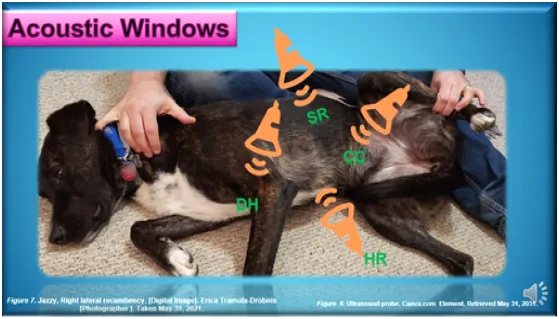
The acoustic windows
For aFAST scans, 4 acoustic windows allow evaluation of the abdomen, providing valuable information; think 30 seconds per site.2,4,7,8
DH view: Diaphragmatic-Hepatic view – Recommended starting point
- Just caudal to the xiphoid
- Fluid sits between the diaphragm and the liver lobes
- The patient can be standing, sternal or lateral for this evaluation. For small effusions, fluid will be most evident in right lateral recumbency
- This view also provides a window into the thoracic cavity allowing visualization of fluid around the pericardium or in the lungs
SR View: Spleno-Renal view
- Left gravity-dependent view
- Over the left flank
- This view allows visualization of the left kidney and spleen
CC view: Cysto-Colic view
- Start the scan just cranial to the bladder
- Allows identification of the colon, bladder, and, if present, the uterus
HR view: Hepato-Renal view
- Scanning occurs just below the belly-button
- Right gravity-dependent view
- Here, we evaluate the area between the body wall and the intestines for free fluid
- Identify and evaluate the liver and the right kidney
- When your patient is lateral, this area represents the most gravity-dependent space
Now you have performed your scan. When performing the evaluation for the assessment of free fluid, we consider the test positive when we have found free fluid in any of the four quadrants. The two most common sites associated with identifying fluid are the CC and DH views.2,8
When scanning, think of the windows as if you are looking at a clock face. Start at the DH view (12:00); then shift to 3:00, the SR view; then 6:00 with the CC view, concluding at 9:00 and the HR view.
Abdominal Fluid Score (AFS)2,5,8
When assessing blunt force trauma, a validated (in right lateral recumbency only) Abdominal Fluid Score (AFS) represents the severity of the trauma and aids in patient monitoring.
Each of the four scanning windows receives a point when fluid is identified. Thus, an AFS of zero means no fluid was detected, while a fluid score of four demonstrates fluid observed in all four quadrants.
When evaluating a trauma patient, identifying an AFS score of 1-2 suggests significant injury but usually represents small-volume bleeders. Thus, these patients are at minimal risk for the development of anemias.
Contrast this with patients receiving AFS scores of 3 or 4. We then have concern for large vessel bleeding and a chance of anemia. Pachtinger and Lisciandro2,5 note that up to 25% of patients with large-vessel bleeders may require transfusion(s).
However, while the number of fluid quadrants helps identify the trauma’s severity, the actual quantity of fluid seen at any acoustic window will not affect the AFS score nor determine severity.3
Patient positioning8
A pet’s position plays a role in identifying fluid and other structures. However, whatever is most comfortable for the animal must ultimately work for you. The pet’s injuries, clinical signs, and even disposition all play a role in what position you will need for that individual patient.
Ideally, the right lateral is preferred by several authors2,4,5 as it can permit access to the chest using the DH view, though fluid detection rates appear equivocal in either lateral position.7 However, Schmidt3 points out that sternal or either lateral recumbency can be utilized for an aFAST scan.
High cost vs. low cost spays and neuters: What’s the difference?
Obstacles and constraints
Remember, an aFAST scan is still just one tool in our toolbox.
Constraints to the effectiveness of an aFAST scan include common limitations and stumbling blocks. By remaining consistent and practicing, one can prevail over common pitfalls. Establishing a set routine and following a systematic protocol helps alleviate common mistakes. Still, issues can arise, including
- Over diagnosing – You don’t want to make definitive life-altering diagnoses for a possible abdominal mass, for example, without obtaining confirmation either via a specialist or additional diagnostics
- Differentiating fat vs. exudates with high cellular content can be challenging
- Failing to see an organ completely, only seeing the “fluid” within a viscera could falsely suggest the presence of free fluid2,4
- When used with hospitalized patients, failing to properly track the fluid serially over time can prevent timely identification of worsening disease, fluid overload, or other developing conditions2,4,5
- Care must be used when applying pressure with the transducer
Too much pressure could displace the fluid leading to a false negative diagnosis
Too little pressure could lead to failure to identify deeper structures or completely view an organ or lesion
An aFAST3 scan’s ability to provide key diagnostic information can be limited by2,7
- The ultrasound machine quality, age, and abilities
- Stressed patients
- When done emergently – lack of quiet and not turning down the lights sufficiently
- Operator proficiency
- Simply identifying the fluid doesn’t allow for its characterization, warranting abdominocentesis. However, if you do that tap and get a syringe of blood, think about how powerful that syringe is when you talk to the owner about your findings and concerns.
- While documented evidence shows high sensitivity in blunt force trauma, this isn’t the case for penetrating traumas. However, even in those instances, aFAST3 scans still have merit by using them for serial evaluations.
- When dehydration and or hypotension exists, fluid may be missed due to rapid reabsorption and vasoconstriction
Practice, practice, practice
As with any skill, performing a diagnostic aFAST scan requires practice. Developing mastery takes time, and using it regularly becomes paramount.
You can consider offering it as a courtesy during your geriatric well-visits at the beginning of your training. This will allow you to gain experience, provide your clients with a perk (free of charge), help you identify abnormalities before they manifest into clinical signs, and enable you to gain proficiency, hone your speed, and learn.
Once you feel you are proficient, charge appropriately for your services.
Always remember that even for those with honed skills and 100% confidence, aFAST scans never take the place of a complete ultrasound. Additional diagnostics and referral to confirm findings to a specialist should always be considered and offered to your clients. You wouldn’t want to condemn a pet to a diagnosis of a mass that ended up being an artifact.
Regardless of how you choose to use this skill, it can be invaluable by providing a source of added income, as a diagnostic tool, to guide additional investigative paths before referral, and as a means to help your patients and provide pet parents with immediate answers.
Various training options are available online and in person for aFAST training. Additional evaluations can be done from tFAST scans to Vet Blue® to Global Fast® and more. Training is paramount to allow practice and help you discern false negatives and positives and possible artifacts that may arise during scanning.
Final food for thought2,8
Reach for that ultrasound probe for the obvious blunt force trauma patient and other common emergencies where warranted. Utilize it in patients with anemias and any post-op or post-intervention patients at risk for bleeding. Finally, use it with penetrating traumas, knowing that the AFS isn’t validated and may prove unrewarding in the acute trauma stage.
But don’t forget to use the technique even if overt free fluid doesn’t even make your initial differential list.
Think about it when you have breeds with certain tendencies towards effusions, those large breed dogs with hemangiosarcomas. Consider it in patients with non-specific, vague, even chronic signs and in patients with collapse or weakness even if normal upon physical exam.
Remember, just taking two minutes to perform the scan can make your job easier, more successful, even more lucrative, and most important, allow you to provide better patient care.
Erica Tramuta-Drobnis, VMD, MPH, CPH is the Founder & CEO ELTD of One Health Consulting, LLC, as well as a freelance writer, consultant, researcher, public health professional and small animal veterinarian.
More from IndeVets:
5 reasons to switch from ER to GP relief
What to do if you find a kitten
Treating FIC with Dr. Erin: A how-to
Your top 5 questions about relief work, answered
References
- Lisciandro GR. Abdominal and thoracic focused assessment with sonography for trauma, triage, and monitoring in small animals. Journal of Veterinary Emergency and Critical Care. 2011;21(2):104-122. doi:10.1111/j.1476-4431.2011.00626.x
- Lisciandro GR. Point-of-Care Ultrasound Techniques for the Small Animal Practitioner, 2nd Edition | Wiley. First. John Wiley & Sons, Incorporated; 2014. Accessed July 21, 2022. https://www.wiley.com/en-us/Point+of+Care+Ultrasound+Techniques+for+the+Small+Animal+Practitioner%2C+2nd+Edition-p-9781119460985
- Schmidt DM. Abdominal Focused Assessment with Sonography for Trauma. Clinician’s Brief. Published 2016. Accessed July 21, 2022. https://www.cliniciansbrief.com/article/abdominal-focused-assessment-sonography-trauma
- Lee J. Emergency Medicine/Toxicology. In: Emergency Medicine/Toxicology. Delaware Valley Academy of Veterinary Medicine; 2020.
- Pachtinger GE. AFAST3 for you and me. DVM 360. Published June 30, 2015. Accessed July 21, 2022. https://www.dvm360.com/view/afast3-you-and-me
- Boysen SR, Rozanski EA, Tidwell AS, Holm JL, Shaw SP, Rush JE. Evaluation of a focused assessment with sonography for trauma protocol to detect free abdominal fluid in dogs involved in motor vehicle accidents. Journal of the American Veterinary Medical Association. 2004;225(8):1198-1204. doi:10.2460/javma.2004.225.1198
- Hammel PE, Berry CR. Sonography Assessment: Overview of AFAST and TFAST. Today’s Veterinary Practice. Published November 2, 2018. Accessed July 21, 2022. https://todaysveterinarypractice.com/radiology-imaging/sonography-assessment-overview-of-afast-and-tfast/
- Tramuta-Drobnis EL. The Usefulness of an aFAST3 Exam as a Point-of-Care Test. In: ER Fast Scan Mastery. First. Vet Ultrasound Training. Scan School Vet Ultrasound Training; 2020:Abdominal fast scan what’s the deal? Accessed June 2, 2021. https://vetultrasoundcourse.com/members-area-access1606238229299
- Tramuta-Drobnis EL. The Usefulness of an aFAST3 Exam as a POC test Published to YouTube. PowerPoint Presentation with Audio presented on June 2, 2021; Online. https://youtu.be/3eHRKKvEZuk